Radiation therapyThe use of high-energy radiation from X-rays, gamma rays, neutrons, protons, and other sources to kill cancer cells and shrink tumors (also known as radiotherapy) is a type of cancer treatment that uses high-powered energy beams. The type of energy that is most commonly used is X-rays, but other types of radiation may be used as well.
Radiation is aimed directly to kill cancer cells and shrink tumorsAn abnormal mass of tissue that results when cells divide more than they should or do not die when they should in the path of the energy beams while doing the least damage possible to the surrounding healthy tissue. Radiation therapy is used in a number of ways. How it is used depends on the patient’s type and stageThe extent of cancer in the body of cancer, the patient’s health status in general, and other factors. In lung cancer, radiation therapy may be used for treatment of both non-small cell lung cancer (NSCLC)A group of lung cancers that are named for the kinds of cells found in the cancer and how the cells look under a microscope; the three main types are lung adenocarcinoma, squamous cell lung cancer, and large cell lung cancer and small cell lung cancer (SCLC)An aggressive (fast-growing) lung cancer that can spread to other parts of the body; the cancer cells look small and oval-shaped through a microscope.1,2,3,4,5,6
Hear more about radiation therapy and lung cancer survivor Jill Feldman's treatment experience.
Radiation therapy has been used as a cancer treatment for more than a century. However, in recent years, technological innovations in engineering and software development have led to significant advances in safety, precision, and effectiveness. Today, radiation therapy is safer and more effective than ever before, and it remains an important option among lung cancer therapies, which may also include surgery, chemotherapyTreatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing, targeted therapiesA type of treatment that uses drugs to identify and attack specific types of cancer cells with less harm to normal cells, angiogenesis inhibitorsDrug given during cancer treatment to prevent the growth of new blood vessels that tumors need to grow, and immunotherapyA type of therapy that uses substances to stimulate or suppress the immune system to help the body fight cancer, infection, and other disease. Each of these treatments attacks lung cancers in different ways.
Radiation therapy may be used alone or in combination with other treatments. After the patient is diagnosed with cancer, a group of healthcare professionals with expertise in that type of cancer commonly get together to discuss what is best for a patient; they help select the optimal treatment plan, which may or may not include radiation therapy. For patients with lung cancer, this group of professionals may include medical oncologists (cancer doctors who specialize in drug therapy), radiation oncologists (cancer doctor who specialize in radiation therapy), thoracic surgeonsSurgeons who have special training in operating on organs inside the chest, including the heart and lungs, lung cancer nurses, pulmonologistsDoctors who have special training in diagnosing and treating diseases of the lung, and others.
Who is on the radiation therapy team, and what are their roles?
The radiation oncology department of any clinic or hospital is staffed by a team of professionals who have specialized training in delivering radiation therapy. This team works together to determine and administer the safest and most effective treatment plan for the patient’s care. Key team members include:7,8,9,10,11
- Radiation oncologist: The radiation oncologist has overall responsibility for the patient’s radiation therapy treatment. The radiation oncologist meets with the patient for a lengthy initial consultation to fully understand the patient’s medical history and complete a medical examination. The radiation oncologist also works with the patient’s other doctors, as needed, to gather any additional necessary medical information. The goal of the initial visit is to determine whether the patient might be a candidate for radiation therapy and what type of treatment might be best. The radiation oncologist develops and prescribes the radiation therapy plan, makes sure that the treatment is given accurately, monitors the patient’s progress, and adjusts the plan as necessary to make sure it is the most effective plan possible. The radiation oncologist continues to meet regularly with the patient and coordinates care with the patient’s other cancer doctors.
- Radiation therapist: The radiation therapist is a highly specialized member of the radiation therapy team who understands how the treatment machines work. The radiation therapist oversees the radiation treatments and makes sure that the prescribed treatments are delivered correctly. The radiation therapist also lets the radiation oncologist know if the patient is experiencing any problems with the treatment.
- Radiation oncology nurse: The radiation oncology nurse provides care for all patients undergoing radiation therapy, including care and support that is needed before, during, and after radiation therapy treatments. The radiation oncology nurse is there to answer any questions, monitor the patient’s health, and help manage any side effects, and works very closely with the radiation oncologist.
- Medical physicist: The medical physicist provides quality control of the radiation equipment and the radiation treatment procedures. The medical physicist ensures that the equipment is properly working by conducting regular safety tests that include measuring the radiation beam itself. The medical physicist works closely with all members of the radiation therapy team. While patients may not meet the medical physicist, he or she plays a critical role on the team.
- Dosimetrist: The dosimetrist is a computer specialist who helps create radiation therapy treatment plans for the radiation oncologist. The dosimetrist works directly with the medical physicist and radiation therapist to calculate the proper dose of radiation given to the patient. As with the medical physicist, patients may not meet the dosimetrist, but he or she plays a critical role on the team.
There are additional members of a patient’s healthcare team who may assist in a patient’s care during treatment, including social workers, nutritionists, and physical therapists.
How does radiation therapy work?
Radiation therapy works by damaging the cancer cells’ ability to grow and multiply; it attacks the DNAThe molecules inside cells that carry genetic information and pass it from one generation to the next. Also called deoxyribonucleic acid within the cells that control these functions. When the cancer cells die, the body naturally eliminates them. Unlike systemic chemotherapy, which kills cancer cells wherever they are throughout the body, radiation only kills cancer cells at which it is aimed. It does not treat any cancer cells that may have spread elsewhere. At times, some cancer cells may survive radiation therapy and need more treatment.

Regardless of the number of doses of radiation a patient receives, radiation therapy does not work immediately, and it varies in its effectiveness by patient. It takes days or weeks before the damage to the DNA is enough for the cells to die. The treatment then continues to work; cancer cells continue to die for up to months after the treatment ends.12,13,14
Radiation therapy can cause side effects. Side effects and their management are discussed later in this section.
What happens at initial consultations with a radiation oncologist?
Radiation therapy does not begin right after the patient meets with the radiation oncologist for the first time. After the first consultation, the radiation oncologist conducts a physical exam, takes a medical history (including a review of medical records, scans, and pathology reports), and may order additional imaging tests, such as X-rays, MRI scans, CT scans, and/or PET scans to get a better idea of the location and extent of the cancer. A follow-up appointment to review the results of any additional tests will be held.
The radiation oncologist may need anywhere from a few days to several weeks to design the patient's treatment plan. The radiation oncologist then reviews the radiation treatment plan with the patient and discusses the potential side effects, where the plan fits into the patient's overall treatment plan, and how the patient can take the best possible care of himself/herself both during and after treatment. This discussion may include a palliative care plan to prevent and ease the potential side effects of treatment.14,15,16
The type of radiation therapy recommended determines the next steps in the process.
How is radiation therapy administered?
Radiation can come from a machine outside the body (external beam radiation therapy, or EBRT) or from radioactive material placed inside the body (internal radiation therapy). Before any radiation treatment is decided on, the radiation oncologist considers a number of factors.
External Beam Radiation Therapy (EBRT)
When radiation therapy is directed at the lung cancer from outside the body, it is called external beam radiation therapy (EBRT). This is the type of radiation therapy most often used to treat both NSCLC and SCLC. The radiation machine used most often is a linear accelerator, also known as a "linac."5,6,17
EBRT procedure
Simulation before radiation treatments begin

Before EBRT is started, there is a planning session that the patient needs to attend following the initial consultations with the radiation oncologist; this is known as simulation. During the simulation, measurements are taken, often with a CT scan, to generate a three-dimensional (3-D) image of the patient's body and the cancer to determine the proper way to give the radiation therapy. There are many decisions that the radiation oncologist needs to make prior to starting the therapy, including the selection of the correct angles for aiming the radiation beams, what dosage to prescribe, and over how many days the radiation doses will be administered. The patient may be fitted with a body mold that restricts movement. The mold helps ensure that the patient stays immobilized and maintains the same position for each treatment. It also ensures patient comfort. Small dots (which can be either temporary or permanent) are put on the patient's skin to serve as guides so that the radiation beams are properly aligned for each radiation therapy treatment session.3,5,6,13,14
When do the radiation treatments actually begin following the simulation?
Radiation treatments do not begin right after the simulation. The radiation therapy start date may be from several days to two weeks after the simulation. It takes this much time for the medical physicist and dosimetrist to create a customized treatment plan that is safe and effective. There are a number of safety checks that have to occur, including confirmation of the calculations that are required by the linear accelerator. Treatments start only after the radiation oncologist gives final approval.18,19
What happens during radiation treatments?
During each treatment, radiation beams are targeted at the marked area on the patient's body. The machine is large and can be noisy (typically a buzzing sound) when it is rotating around the patient delivering the radiation from different angles, but the machine never touches the patient's body. Radiation therapy is painless. Each session lasts 5-30 minutes. Most of this time is spent positioning the body to make sure that the beam is aligned with the targeted area defined by the radiation oncologist. 5,6,13,14

Doctors use the term GY (gray) to describe the dose of radiation therapy. Gy is the new international system unit of radiation dose expressed as absorbed energy per unit mass of tissue.20
A radiation therapy schedule usually consists of a specific number of treatments given over a set period of time. The schedule varies by circumstance, including the stage of lung cancer, the type of radiation therapy, and the goal of the radiation therapy. For example, a course for stage II or stage III lung cancer could consist of sessions 5 days per week (Monday-Friday) for 6 to 7 weeks, for a total of 30 to 35 treatments, but even this may vary. In addition to these weekly radiation sessions for stage II or stage III NSCLC, the patient has a weekly meeting with the radiation oncologist and oncology nurse. These are called on-treatment visits, or OTVs. At the OTV, the patient can be assessed for side effects from treatment, and any other concerns are discussed. The OTV takes place even when the patient is feeling well. Based on the radiation oncologist's appraisal at the OTV, the patient's treatment plan may be adjusted.5,6,13,20,21,22,23
After the radiation treatments have ended, the patient continues to see the radiation oncologist for follow-up observation and care; the radiation oncologist determines how often and for how long this will be necessary.21,22
Types of EBRT
The radiation oncologist determines which EBRT technique may be the most effective for a patient. Among these techniques are:
- Three-dimensional conformal radiation therapy (3D-CRT): 3D-CRT uses imaging technology (CT, MRI, PET, or PET-CT) to generate 3D images of a patient's tumor and the surrounding area. This level of detail allows for a stronger dose of radiation to be administered to the tumor while causing less damage to the normal, healthy tissue around the tumor. 3D-CRT is used for tumors that are shaped irregularly or that are positioned close to healthy organs or tissue.5,6,,24,25,26,27
-
Intensity-modulated radiation therapy (IMRT): IMRT also uses three-dimensional imaging. Coordinates of the tumor from the imaging are used to program a machine that can then deliver, from multiple angles, precisely shaped and higher doses of radiation to the tumor and lower doses to the surrounding normal, healthy tissue. Because it is so precise, IMRT is an especially useful technique for use when a tumor is situated near a vital structure, such as the spine.5,6,25,28,29,30

-
Stereotactic body radiation therapy (SBRT): SBRT, also called stereotactic ablative radiotherapy (SABR), combines image-guided radiation therapy (IGRT) with even more advanced techniques to precisely deliver extremely high doses of radiation to the tumor while decreasing the dose to normal, healthy tissue nearby. Instead of giving small doses of radiation each day for several weeks, SBRT can be given in two to five treatments. When the treatment is delivered in only one session, it is referred to as stereotactic radiosurgery (SRS). In lung cancer, SBRT is most often used to treat early-stage NSCLC when the patient's health does not allow surgery or the patient does not want surgery. It can be used for tumors small in size (5 cm or less). It may also be used if an NSCLC patient has limited metastases.3,5,31,32,33
-
Proton therapy: Proton therapy is a type of radiation therapy that uses protonsSmall, positively charged particles of matter found in the atoms of all elements instead of X-rays to treat cancer. Like X-rays, the proton beam damages the DNA within the cancer cells, leading to the cells' death. As with the other radiation therapy, imaging is done to determine where exactly the radiation needs to be targeted. The machine used, known as a cyclotron or synchotron, propels the protons at high speed. The main advantage of proton therapy is that all of the radiation is released when it gets to the tumor, so radiation damage to the normal, healthy tissue in the area is lessened; this may allow a higher radiation dose to be given to the tumor. However, proton therapy is very expensive and is not covered by all insurance companies for all diagnoses. In addition, it requires expensive and specialized equipment that only a handful of hospitals in the United States have.34,35
| 3D-CRT | IMRT | SBRT | Proton Therapy | |
| When is it used? | Stage II-IV | Stage II-IV | Stage I or IV | Stage I-IV |
| When is it not used? | Most palliative treatments | Whenever tumors are very close to critical body structures | Most palliative treatments | |
| Main difference | Easiest type of radiation to deliver; less technical expertise required | Dose of radiation is shaped more conformally around tumor compared with 3D-CRT | Very high doses in a few fractions with sharp dose gradients; leads to higher rates of local control of the cancer | Reduces volume of tissue receiving low doses |
Internal Radiation Therapy
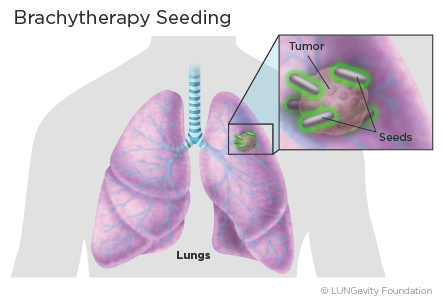
The other type of radiation therapy is internal radiation therapy. Internal radiation therapy is used for lung cancer treatment only in situations when the radiation oncologist recommends a high dose of radiation in a small area, such as in the airway. This type of internal radiation therapy is called brachytherapy. During treatment, a small source of radioactive material, often in the form of small pellets or seeds, is inserted directly into the cancer or into the airway next to the cancer. This is usually done during a bronchoscopyA procedure that uses a thin, tube-like instrument with a light and a lens to examine the inside of the trachea, bronchi, and lungs or during surgery. The radiation travels only a short distance from the implanted radiation source to the tumor, which limits damaging effects on surrounding normal, healthy tissue. The radioactive material may be removed after a short time—several minutes for high-dose-rate brachytherapy or up to a few days for low-dose-rate brachytherapy. Alternately, radioactive seeds my be left in place permanently; the radiation gets weaker over time until it is no longer radioactive.5,12,14
Radiation therapy safety
EBRT does not make patients radioactive, so a patient cannot transmit radiation to anyone else. However, a patient who is treated with internal radiation therapy implants can emit radiation to other people; the radiation oncologist advises the patient about what precautions should be taken.14,17,36,37,38
All forms of radiation therapy carry a very small risk of developing a second cancer. The risk is typically one in 5,000 patients.39
Goals of radiation therapy in lung cancer treatment
The overarching goal of radiation therapy in lung cancer treatment is to stop the growth of tumors while keeping the risk of side effects from toxicity due to the treatment to a minimum. As with all radiation therapy, how it is specifically used to treat lung cancer depends on the patient's type and stage of lung cancer, overall health and other medical factors, and other personal considerations. The radiation oncologist discusses the specific goals of the radiation therapy with the patients and may discuss how it can be combined with surgery and/or chemotherapy, targeted therapy, or immunotherapy. Typical strategies for radiation therapy include:1,23,4,5,6,40,41,42,43,44
- As the patient's primary treatment, with or without intent to cure
- Before surgery, with or without chemotherapy, to reduce the size of a tumor
- After surgery, with or without chemotherapy, to kill any remaining cancer cells
- To treat areas where lung cancer has spread outside of the lungs, such as the brain and bones
- As a treatment to one area that is progressing when targeted therapy or immunotherapy is controlling other sites of disease
- To relieve symptoms, such as pain or shortness of breath, by shrinking the tumor
How radiation therapy fits into lung cancer treatment plans
Radiation therapy may potentially be used at all stages of both NSCLC and SCLC, alone or in combination with other treatments. The following treatments described are most commonly used; there may be other treatments recommended by the radiation oncologist that are not listed here as well as new treatment approaches being tested in clinical trialsA type of research study that tests how well new medical approaches work in people. More information about clinical trials can be found here.
Non-small cell lung cancer (NSCLC)
Radiation therapy for NSCLC is usually given five days a week for five to seven weeks, but this can vary based on the type of EBRT being used, the stage and location of the NSCLC, and the intent of the radiation therapy. The following table shows, for example, how SBRT can be used for the treatment of NSCLC based on the location and size of the tumor.5,41
| Total Dose | Total # of Fractions | Size and Location of Lung Tumor |
| 25-34 Gy | 1 | Peripheral, small (<2 cm) tumors, especially >1 cm from chest wall |
| 45-60 Gy | 3 | Peripheral tumors and >1 cm from chest wall |
| 48-50 Gy | 4 |
Central or peripheral tumors <4 -5 cm, especially <1 cm from chest wall |
| 50-55 Gy | 5 |
Central or peripheral tumors, especially <1 cm from chest wall |
| 60-70 Gy | 8-10 |
Central tumors |
Early-stage NSCLC (stages I and IIA with no spread to lymph nodes)
While the other types of EBRT may be used, SBRT is often recommended for early-stage patients (stages I and IIA with no spread to lymph nodesSmall bean-liked structures that are part of the body's immune system. They contain lymphocytes, which help the body fight infection and disease who either cannot or choose not to have surgery. It is an option for patients who have high surgical risk, possibly because of advanced age or poor lung function. For patients who have had surgery, EBRT following surgery is recommended when the margins of the removed cancer indicate that there are remaining cancer cells. In some cases, chemotherapy may be recommended after radiation.41,45
Locally advanced NSCLC (stages II and III)
Radiation therapy for stages II and III lung cancer is typically delivered with concurrent chemotherapy (chemotherapy and radiation given at the same time). At times, surgery may be an alternative option and both are typically recommended for cure. In patients who cannot tolerate the potential side effects of concurrent radiation and chemotherapy, the chemotherapy may be given before radiation therapy, or radiation therapy may be given without any chemotherapy at all.41
Among stage III NSCLC patients whose cancer has not grown after cycle 2 following chemoradiation, the immunotherapy drug durvalumab (Imfinzi®), a PD-L1 checkpoint inhibitor, may be administered to help prevent progression and has been shown to improve survival. Durvalumab is given by infusion every two weeks until the cancer starts growing or for a maximum of 12 months.46
Advanced/metastatic NSCLC (Stage IV)
In stage IV NSCLC with extensive metastasesCancer cells that have spread from the place where they first formed to other parts of the body, radiation therapy, both EBRT and brachytherapy, can be used to relieve or prevent symptoms of lung cancer, such as pain or obstruction of an airway.
At times, it may be used to treat oligometastases, which are a small number of metastatic lesions found at limited sites. SBRT is often considered an option for this if it can safely be administered.42,43,44
Patients with brain metastases have several radiation therapy options. Those with limited metastases may be treated with SRS (e.g., using the Gamma Knife® technology), in which precisely targeted beams deliver high doses of radiation to the metastases. The other radiation therapy option is whole-brain radiation therapy, in which radiation is given to the whole brain. It is not yet clear whether one technique has a survival benefit over the other, but the side effects may be lessened with SRS.47

In some situations, brain metastases may be treated with targeted therapies and not require radiation.
Small cell lung cancer (SCLC)
Limited-stage small cell lung cancer (LS-SCLC)
EBRT is often prescribed for limited-stage non-small cell lung cancer (LS-SCLC)Small cell lung cancer (SCLC) found in one lung, the tissue between the lungs, and nearby lymph nodes only with a goal of complete tumor eradication and long-term cure. It is often delivered with concurrent chemotherapy. Chemotherapy may begin at the same time or shortly before radiation therapy begins. The radiation therapy treatments may be delivered once daily for six to seven weeks or twice daily for three weeks. Patients and doctors often decide on the once- vs twice-daily schedule based on convenience and preference, as it is generally not thought to make a difference to the long-term probability of tumor control. There are no other major differences in side effects or treatment efficacy between once-daily and twice-daily radiation treatments, as shown in a large trial conducted in Europe comparing these two dosing schedules.39,48
Certain patients with an LS-SCLC diagnosis who either cannot or choose not to have surgery may be treated specifically with SBRT, followed by chemotherapy.
In patients with LS-SCLC who have responded well to their initial treatment, prophylactic cranial irradiation—radiation to the brain—may be used to prevent brain metastases.48
Extensive-stage small cell lung cancer (ES-SCLC)
EBRT cannot completely eradicate all sites of cancer in patients with extensive-stage small cell lung cancer (ES-SCLC)Small cell lung cancer (SCLC) that has spread outside the lung in which it began or to other parts of the body. However, it can be used after chemotherapy to improve control of disease in areas that are predicted to relapse. It may also be prescribed to the whole brain to reduce the risk of brain metastases and neurological complications. EBRT can also be used to help control symptoms that chemotherapy cannot help, such as pain, breathing problems, or bleeding.39,48
What is the abscopal effect?
Radiation therapy kills cancer cells. Dying cells release proteins and attract immune cells, leading to immune cell activation. The addition of immunotherapy can boost this immune response. This immune activation can have an effect on distant organs by killing cancer cells at distant sites. This is referred to as the abscopal effect.49

Managing radiation therapy side effects
Side effects from radiation therapy are caused by the damage to the normal, healthy cells that are near the cancer cells that are being treated. One major advantage of the more precise radiation therapy techniques that have been developed is that a smaller area of the normal, healthy tissue is damaged, which decreases the risk of side effects.
Side effects from radiation therapy for lung cancer are common, but just because a side effect is common does not mean that a patient will experience it. Before treatment begins, a patient should discuss with the radiation therapy team what side effects might be expected and how to prevent or ease them with a palliative care plan. Radiation oncologists check in weekly with each patient undergoing treatment to assess if any side effects are occurring. However, patients who are experiencing problems should speak with the radiation therapy team as soon as possible whenever a new side effect begins. This is because treating side effects early on is often more effective than trying to treat them after they have become severe. Although most radiation therapy side effects go away when treatment is over, some can last a long time or even be permanent. It is important to know that a new side effect may occur even after treatment is over.
The side effects and management techniques listed below are not all-inclusive. The radiation therapy team will have a more comprehensive list of side effects that might be expected given the type of radiation being used and can offer the patient a personalized set of recommendations for their management. They can also offer tips for caregivers.
Most side effects begin during the second or third week of treatment. Common side effects of radiation therapy and ways to manage them include:2,5,14,50,51
- Fatigue: Fatigue can be treated with plenty of sleep, rest between activities, exercise, relaxation techniques (eg, medication or yoga), good nutrition, and treatments (if appropriate) for anemia or depression. Another major cause of fatigue from radiation is dehydration. Patients should make sure to get plenty of fluids during radiation treatments (more than what they would take in normally), as this wil markedly help.
- Sunburn-like skin changes, such as dryness, itching, or peeling: Symptoms may be relieved by washing with gentle soap and warm water (not hot) and using unscented creams/lotions.
- Hair loss: Hair will only fall out in the area where the radiation enters the body. If radiation therapy is only to the chest area, for example, there will be no loss of hair on the head.
- Cough, difficulty breathing, and shortness of breath: Many times these symptoms are due to the cancer itself. A cough can sometimes get worse during radiation as the airways develop inflammation. Anti-cough medications can be given to help with this. Inflammation from radiation typically gets better within two weeks after treatment, and many times this symptom will go away as the inflammation goes down. A cough and shortness of breath can sometimes develop as “radiation pneumonitis” up to months after therapy and may require anti-inflammatory medication.
- Sore throat, trouble swallowing, and chest pain: These usually happen because the radiation causes the esophagusThe muscular tube through which food passes from the throat to the stomach to develop inflammation. Pain and anti-inflammatory medications and speech pathology to learn different ways to swallow may help. These symptoms typically get better within two weeks after radiation is completed, but can sometimes persist longer.
- Loss of appetite and weight loss: Appetite stimulants and nutritional supplements may be given to improve appetite and reduce weight loss.
- Nausea and vomiting when the treated area is near the stomach: Bland and easy-to-digest foods and frequent small meals and snacks may help prevent nausea. Techniques such as distraction, relaxation, and positive imagery can help change the expectation and fear of nausea and vomiting. In addition, there are multiple medications available to prevent and treat nausea and vomiting. If one anti-nausea medication does not work, a different one or an additional one can be prescribed.
What's new in lung cancer radiation therapy research?
There are currently clinical trials under way that aim to further improve the precision of imaging and radiation delivery techniques. Researchers are looking into new imaging techniques, and radiation therapy is also being studied in combination with surgery, chemotherapy, immunotherapy, and targeted therapy cells.52 It is important to note that no patient receives less than the current standard of care when participating in a clinical trial.
If you are considering participating in a clinical trial, start by asking your doctor whether there is one for which you might qualify in your area. In addition, there are several resources to help you find one that may be a good match for you.
LUNGevity partners with Carebox, a clinical trials matching service, to help you with the decision of whether to participate in a clinical trial. Carebox helps you identify which lung cancer clinical trials you may be eligible for. The clinical trial navigators can also guide you through the process of getting enrolled if you choose to take part in a clinical trial. Clinical trial navigators are available Monday through Friday from 9:00 am to 5:00 pm ET at 877-769-4834 (in both English and Spanish). Learn more about this free service and even fill out an online profile to help identify clinical trials that might be a good match for you.
Information about available clinical trials is also available through these websites:
- National Cancer Institute clinical trials search: This site includes all of the thousands of clinical trials in the United States in all cancer types.
- My Cancer Genome: This resource is managed by a team of doctors at Vanderbilt University. My Cancer Genome gives up-to-date information on what mutations make cancers grow and related treatment options, including available clinical trials.
- Lung Cancer Master Protocol (Lung-MAP): For patients with advanced non-small cell lung cancer, Lung-MAP is a collaboration of many research sites across the country, using a unique approach to matching patients to one of several drugs being developed.
Updated February 22, 2021
References
- Lung Cancer — Non-Small Cell:Types of Treatment. Cancer.Net website. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/types-treatment. Approved May 2020. Accessed February 22, 2021.
- Lung Cancer Treatment. RadiologyInfo.org. https://www.radiologyinfo.org/en/info.cfm?pg=lung-cancer-therapy#therapy-treatment. Reviewed July 17, 2019. Accessed February 22, 2021.
- Non-Small Cell Lung Cancer. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Version 3.2021. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Posted February 16, 2021. Accessed February 22, 2021.
- Small Cell Lung Cancer. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Version 2.2021. https://www.nccn.org/professionals/physician_gls/pdf/sclc.pdf. Posted January 11, 2021. Accessed February 22, 2021.
- Radiation Therapy for Non-Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/non-small-cell-lung-cancer/treating/radiation-therapy.html. Revised October 1, 2019. Accessed February 22, 2021.
- Radiation Therapy for Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/small-cell-lung-cancer/treating/radiation-therapy.html. Revised October 1, 2019. Accessed February 22, 2021.
- What to Expect When Having Radiation Therapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/radiation-therapy/what-expect-when-having-radiation-therapy. Approved August 2020. Accessed February 22, 2021.
- Radiation Oncology Team. Targeting Cancer website. https://www.targetingcancer.com.au/radiation-oncology-team/. Copyright 2017. Accessed February 22, 2021.
- Professions in Radiation Therapy. RadiologyInfo.org website. https://www.radiologyinfo.org/en/info.cfm?pg=professions-radiation-therapy. Reviewed May 5, 2019. Accessed February 22, 2021.
- What is a Medical Dosimetrist? American Association of Medical Dosimetrists website. https://www.medicaldosimetry.org/about/medical-dosimetrist/. Updated July 2020. Accessed February 22, 2021.
- Meet the Radiation Oncology Treatment Team. Countryside Cancer Center website. https://www.countrysidecancercenter.com/index.php/meet-the-radiation-oncology-team-/. Copyright 2021. Accessed February 22, 2021.
- Radiation Therapy to Treat Cancer. National Cancer Institute website. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy. Revised January 8, 2019. Accessed February 22, 2021.
- Radiation therapy. Mayo Clinic website. https://www.mayoclinic.org/tests-procedures/radiation-therapy/about/pac-20385162. Copyright 2021. Accessed February 22, 2021.
- Radiation Therapy and You: Support for People with Cancer. National Cancer Institute website. https://www.cancer.org/publications/patient-education/radiationtherapy.pdf. Updated 2016. Accessed February 22, 2021.
- New Patient Checklist. University of Florida website. https://radonc.med.ufl.edu/patient-care/appointment-information/new-patient-checklist/. Copyright 2021. Accessed February 22, 2021.
- What is external radiotherapy? Cancer Research UK website. https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/radiotherapy/external/about. Reviewed Noveber 6, 2020. Accessed February 22, 2021.
- Understanding Radiation Therapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/radiation-therapy/understanding-radiation-therapy. Approved August 2020. Accessed February 22, 2021.
- Radiation Oncology— simulation. Weill Cornell Medicine website. https://radiationoncology.weillcornell.org/clinical-services-and-technologies/external-beam-radiation-therapy/simulation. No posting date. Accessed Feburary 22, 2021.
- Step-by-Step Through Treatment. UC Davis website. https://health.ucdavis.edu/radonc/patients/Rx_stepbystep.html. Copyright 2021. Accessed February 22, 2021.
- Gray (Gy). Radiation Emergency Medical Management website. https://www.remm.nlm.gov/gray_definition.htm. Updated october 26, 2020. Accessed February 22, 2021.
- Pictorial Overview of the Radiation Therapy Treatment Process. OncoLink website. https://www.oncolink.org/cancer-treatment/radiation/introduction-to-radiation-therapy/pictorial-overview-of-the-radiation-therapy-treatment-process. Reviewed July 30, 2020. Accessed February 22, 2021.
- What is Radiation Therapy? Beth Israel Deaconess Medical Center website. https://www.bidmc.org/centers-and-departments/radiation-oncology/faqs. Copyright 2021. Accessed February 22, 2021.
- About Your Treatment. Washington University School of Medicine in St. Louis Department of Radiation Oncology website. https://radonc.wustl.edu/patient-care/about-your-treatment. Copyright 2021. Accessed February 22,2021.
- 3D CRT (Three-Dimensional Conformal Radiation Therapy). Moffitt Cancer Center website. https://moffitt.org/treatments/radiation-therapy/3d-crt-three-dimensional-conformal-radiation-therapy/. Copyright 2018. Accessed February 22, 2021..
- Hegi F, Atwood T, et al. Technical Requirements for Lung Cancer Radiotherapy. In: Pass HI, Ball D, Scagliotti GV, eds. IASLC Thoracic Oncology, 2nd ed. Philadelphia, Pa.: Elsevier: 2018: 318-29. Accessed June 25, 2019.
- External beam radiation therapy. Cancer Treatment Centers of America website. https://www.cancercenter.com/treatment-options/radiation-therapy/external-beam-radiation. Copyright 2021. Accessed February 22, 2021.
- 3D & 4D Conformal Radiation Therapy and Intensity Modulated Radiation Therapy (IMRT). The Angeles Clinic and Research Institute website. http://www.theangelesclinic.org/Home/PatientEdcarionLibrary/tabid/19283/ctl/View/mid/35200/Default.aspx?ContentPubID=419. Copyright 2021. Accessed February 22, 2021.
- IMRT (Intensity Modulated Radiation Therapy). Moffitt Cancer Center website. https://moffitt.org/treatments/radiation-therapy/imrt-intensity-modulated-radiation-therapy/. Copyright 2018. Accessed February 22, 2021.
- Image-guided Radiation Therapy (IGRT). RadiologyInfo.org website. https://www.radiololgyinfo.org/en/info.cfm?pg=igrt. Reviewed April 3, 2018. Accessed February 22, 2021.
- IMRT. UCLA Health website. https:/www.uclahealth.org/radonc/imrt-igrt. No posting date. Accessed February 22, 2021.
- FAQs. Stereotactic Body Radiation Therapy (SBRT). UCLA Health website. https://www.uclahealth.org/radonc/faqs-sbrt. No posting date. Accessed February 22, 2021.
- SBRT (Stereotactic Body Radiation Therapy). Moffitt Cancer Center website. https://moffitt.org/treatments/radiation-therapy/sbrt-stereotactic-body-radiation-therapy/. Copyright 2018. Accessed February 22, 2021.
- Non-Small Cell Lung Cancer Treatment (PDQ®)—Patient Version. National Cancer Institute website. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq. Updated December 3, 2020. Accessed February 22, 2021.
- Proton Therapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/radiation-therapy/proton-therapy. Approved August 2018. Accessed February 22, 2021.
- Stallard J. Proton Therapy: A Better Way to Destroy Tumors. Memorial Sloan Kettering Cancer Center website. https://www.mskcc.org/blog/proton-therapy-better-way-destroy-tumors. Posted February 17, 2015. Accessed February 22, 2021.
- Internal Radiation Therapy (Brachytherapy). American Cancer Society website. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/radiation/internal-radiation-therapy-brachytherapy. Revised February 10, 2017. Accessed February 22, 2021.
- Stallard J. Answers to Common Questions about Radiation Safety. Memorial Sloan Kettering website. https://www.mskcc.org/blog/answers-common-questions-about-radiation-safety. Posted May 28, 2020. Accessed February 22, 2021.
- Schlembach P. Radiation therapy: 11 questions my patients ask. The University of Texas MD Anderson website. https://www.mdanderson.org/publications/cancerwise/radiation-therapy--11-questions-my-patients-ask.h00-159146823.html. Posted July 27, 2017. Accessed February 22, 2021.
- Conversation with Drew Moghanaki, MD, MPH. January 26, 2020.
- Radiation Therapy for Non-Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/radiation-therapy.html. Revised October 1, 2019. Accessed February 22, 2021.
- Non-Small Cell Lung Cancer. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). NCCN Evidence BlocksTM. Version 3.2021. Published February 20, 2021. Accessed February 22, 2021.
- Ning MS, Gomez DR, et al. Stereotactic ablative body radiation for oliogmetastatic and oligoprogressive disease. Trans Lung Cancer Res. 2019: 8(1): 97-106. doi: 10.21037/ticr.2018.09.21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6351406/. Accessed February 22, 2021.
- Basier L, Kroeze SG, Guckenberger. SBRT for oligoprogressive oncogene addicted NSCLC. Lung Cancer. 2017; 106:50-57. doi: 10.1016/j.lungcan.2017.02.007. https://www.ncbi.nlm.nih.gov/pubmed/28285694. Published February 6, 2017. Accessed February 22, 2021.
- Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of 4-10 oligometastatic tumors (SABR-COMET-10): study protocol for a randomized phase III trial. BMC Cancer. 2019; 19:816. doi: 10.1106/s12885-019-5977-6. https://euopepmc.org/articles/PMC6699121. Accessed February 22, 2021.
- Lung Cancer: Early and Locally Advanced Non-Small Cell Lung Cancer. NCCN Guidelines for Patients®, Version 3.2019. https://www.nccn.org/patients/guidelines/content/PDF/lung-early-stage-patient.pdf. Published January 18, 2019. Accessed February 22, 2021.
- Imfinzi® (durvalumab). Prescribing Information. AstraZeneca Pharmaceuticals LP: Wilmington, DE. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761069s018lbl.pdf. Revised March 2020. Accessed February 22, 2021.
- Mizuno T, et al. Comparison between stereotactic radiosurgery and whole-brain radiotherapy for 10-20 brain metastases from non-small cell lung cancer. Mol Clin Oncol. 2019; 10(5):560-6. doi: 10.3892/mco.2019.1830. https://www.ncbi.nlm.nih.gov/pubmed/30967951. Published March 20, 2019. Accessed February 22, 2021.
- Conversation with Kristin Higgins, MD. February 17, 2020.
- Widel M. Radionuclides in radiation-induced bystander effect: may it share in radionuclide therapy? Neoplasma. 64, 5, 2017. doi: 10.4149/neo_2017501. https://www.researchgate.net/profile/Maria_Widel/publication/317406778_Radionuclides_in_radiation_induced_bystander_effect_may_it_share_in_radionucli…; Published February 1, 2017. Accessed Feb ruary 22, 2021.
- Side Effects of Radiation Therapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/radiation-therapy/side-effects-radiation-therapy. Approved August 2020. Accessed February 22, 2021.
- Radiation Therapy Side Effects. National Cancer Institute website. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/side-effects. Posted May 1, 2018. Accessed February 22, 2021.
- Clinicaltrials.gov. US National Institutes of Health website. http://clinicaltrials.gov. Accessed February 22, 2021.
